When it comes to our health, there's no such thing as too much information. One of the most insightful ways to understand your body better is through blood testing. It might sound like a scene from a medical drama, but trust me, it's far more mundane and much less dramatic.
Here are 12 compelling reasons to roll up your sleeve and get that blood test done.

1. Understand Your Baseline Health
Imagine starting a road trip without a map – that’s how navigating health without baseline blood work feels. Baseline blood tests provide an invaluable snapshot of your current health, offering detailed insights into your body’s inner workings. This foundational data includes critical biomarkers such as cholesterol levels, blood glucose, and more.
Cholesterol Levels: Cholesterol is a waxy substance found in your blood, essential for building healthy cells but potentially harmful at elevated levels. High levels of low-density lipoprotein (LDL) cholesterol can lead to plaque buildup in arteries, increasing the risk of cardiovascular diseases. A baseline blood test reveals your LDL and high-density lipoprotein (HDL) levels, helping you and your healthcare provider devise strategies to maintain a healthy balance.
Blood Glucose: Blood glucose, or blood sugar, is the primary energy source for your body’s cells. Maintaining optimal blood glucose levels is crucial, as persistently high levels can indicate prediabetes or diabetes, conditions that necessitate immediate attention and management. Baseline blood testing identifies your fasting blood glucose and hemoglobin A1c (HbA1c) levels, providing a comprehensive view of your glycemic control over the past few months.
Liver and Kidney Function: Your liver and kidneys play vital roles in detoxifying your body, processing nutrients, and filtering waste. Baseline blood tests measure liver enzymes (such as ALT and AST) and kidney function markers (like creatinine and blood urea nitrogen) to ensure these organs are functioning optimally. Early detection of any anomalies can lead to prompt intervention, potentially averting serious health issues.
Complete Blood Count (CBC): A CBC is a comprehensive test that evaluates the overall health of your blood cells. It measures red blood cells, white blood cells, hemoglobin, hematocrit, and platelets. This test can detect a range of disorders, including anemia, infections, and hematologic diseases. Understanding these parameters can help identify underlying conditions that might not yet be symptomatic.
Inflammation Markers: Chronic inflammation is linked to numerous health issues, including heart disease, diabetes, and autoimmune disorders. Baseline blood tests often include markers like C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR), which indicate inflammation levels in your body. Monitoring these markers helps in assessing your overall inflammatory status and taking preventive measures if necessary.
By establishing a baseline, you create a reference point for future comparisons. Regular blood testing allows you to track changes over time, making it easier to identify trends or deviations from your normal values. This proactive approach enables early intervention, personalized treatment plans, and a better understanding of how lifestyle changes or medications are impacting your health.
Understanding your baseline health through blood tests is like having a detailed roadmap for your health journey. It provides the essential information needed to navigate your way to better health, wellness, and performance, ensuring you stay on the right path towards a healthier future.
2. Identify Nutrient Deficiencies
Are you feeling more sluggish than usual? Experiencing fatigue, mood swings, or decreased cognitive function? These symptoms might be more than just the result of a busy lifestyle; they could indicate nutrient deficiencies. Blood tests are a powerful tool for identifying deficiencies in essential vitamins and minerals, such as iron, vitamin D, B12, and magnesium, which are crucial for maintaining optimal health and energy levels.
Iron: Iron is a critical component of hemoglobin, the protein in red blood cells responsible for transporting oxygen throughout the body. Iron deficiency, or anemia, can lead to symptoms like fatigue, weakness, and shortness of breath. A blood test measuring serum ferritin, total iron-binding capacity (TIBC), and hemoglobin levels can diagnose iron deficiency anemia. Once identified, iron levels can be corrected through dietary adjustments or supplementation, improving oxygen transport and energy levels.
Vitamin D: Vitamin D, often referred to as the “sunshine vitamin,” plays a vital role in bone health, immune function, and mood regulation. Deficiency in vitamin D is surprisingly common, especially in regions with limited sunlight exposure. Symptoms of deficiency can include bone pain, muscle weakness, and increased susceptibility to infections. Blood tests measuring 25-hydroxyvitamin D [25(OH)D] levels provide a precise assessment of your vitamin D status. If deficient, vitamin D levels can be improved through supplementation and increased sun exposure, leading to better overall health and well-being.
Vitamin B12: Vitamin B12 is essential for nerve function, red blood cell production, and DNA synthesis. Deficiency in B12 can cause a range of symptoms, from fatigue and weakness to neurological issues like numbness, tingling, and cognitive disturbances. Blood tests that measure serum B12 levels and methylmalonic acid (MMA) can accurately diagnose a B12 deficiency. Addressing this deficiency typically involves dietary changes, oral supplements, or in more severe cases, B12 injections, which can significantly enhance energy levels and neurological function.
Magnesium: Magnesium is involved in over 300 biochemical reactions in the body, including muscle and nerve function, blood glucose control, and bone health. A deficiency in magnesium can manifest as muscle cramps, mental disturbances, and cardiovascular issues. Blood tests measuring serum magnesium levels can help identify deficiencies. Correcting low magnesium through dietary sources like nuts, seeds, and leafy greens or through supplementation can improve muscle function, reduce cramps, and enhance overall metabolic health.
Zinc and Selenium: Zinc and selenium, though needed in trace amounts, are essential for immune function, thyroid health, and DNA synthesis. Deficiencies in these minerals can lead to a weakened immune response, thyroid dysfunction, and reproductive issues. Blood tests can measure serum levels of these trace elements, and supplementation or dietary adjustments can restore optimal levels, supporting immune health and metabolic function.
Folate (Vitamin B9): Folate is crucial for DNA synthesis, repair, and methylation, as well as red blood cell production. Deficiency in folate can cause megaloblastic anemia, leading to fatigue, pallor, and shortness of breath. Blood tests measuring serum folate levels can diagnose a deficiency. Increasing dietary intake of folate-rich foods like leafy greens, legumes, and fortified cereals, or taking supplements, can correct this deficiency, improving red blood cell production and overall health.
By revealing deficiencies in these essential nutrients, blood tests empower you to make informed decisions about your diet and supplementation. Addressing these deficiencies can lead to significant improvements in energy levels, cognitive function, immune health, and overall well-being.
In essence, understanding and correcting nutrient deficiencies through blood tests is like fine-tuning the engine of a high-performance car. With the right balance of vitamins and minerals, your body can operate at peak efficiency, ensuring you feel your best every day.
3. Monitoring Chronic Conditions
For those living with chronic conditions such as diabetes, hypertension, or hyperlipidemia, regular blood tests are not just a health check-up—they are a lifeline. These tests play a crucial role in monitoring the effectiveness of treatments, adjusting medications, and ensuring that critical health markers remain within target ranges. By keeping those pesky numbers in check, patients can maintain a better quality of life and potentially avoid severe complications.
Diabetes
In diabetes management, regular blood tests are indispensable. The primary markers monitored include:
- HbA1c (Glycated Hemoglobin): This test provides an average of your blood glucose levels over the past 2-3 months. It’s a reliable indicator of long-term glucose control. Maintaining an HbA1c level below the target range (usually 7% for most patients) helps prevent complications such as neuropathy, retinopathy, and nephropathy.
- Fasting Blood Glucose: This test measures blood sugar levels after an overnight fast. Elevated fasting glucose levels can indicate poor glucose control and the need for treatment adjustments.
- Lipid Profile: Diabetes often coexists with dyslipidemia, increasing the risk of cardiovascular disease. Regular lipid profiles measure total cholesterol, LDL, HDL, and triglycerides, helping to manage cardiovascular risk factors.
- Kidney Function Tests: Diabetes can damage the kidneys over time, leading to nephropathy. Monitoring serum creatinine and urine albumin levels helps assess kidney function and catch early signs of damage.
Hypertension
High blood pressure, or hypertension, is a significant risk factor for heart disease and stroke. Blood tests in hypertension management often include:
- Electrolyte Panel: This panel measures sodium, potassium, and other electrolytes to ensure they remain within normal ranges, especially since some antihypertensive medications can affect electrolyte balance.
- Kidney Function Tests: Elevated blood pressure can damage the kidneys. Monitoring serum creatinine and blood urea nitrogen (BUN) levels helps assess kidney health and function.
- Lipid Profile: Since hypertension and high cholesterol often go hand-in-hand, regular lipid profiles help manage overall cardiovascular risk.
Hyperlipidemia
Hyperlipidemia, characterized by elevated cholesterol and triglycerides, significantly increases the risk of cardiovascular disease. Regular blood tests for managing hyperlipidemia include:
- Lipid Profile: Monitoring total cholesterol, LDL, HDL, and triglycerides helps guide dietary and pharmacological interventions to reduce cardiovascular risk.
- Liver Function Tests: Statins, commonly prescribed for hyperlipidemia, can affect liver enzymes. Regular monitoring ensures these medications are not adversely impacting liver function.
Thyroid Disorders
Thyroid conditions, such as hypothyroidism and hyperthyroidism, require regular blood tests to monitor hormone levels and adjust medications:
- Thyroid Stimulating Hormone (TSH): This test measures the pituitary hormone that stimulates the thyroid. Abnormal TSH levels can indicate the need to adjust thyroid medication dosages.
- Free T4 and Free T3: These tests measure the levels of active thyroid hormones in the blood, providing a more detailed picture of thyroid function.
Liver Disease
For patients with chronic liver conditions, regular blood tests are essential to monitor liver health and function:
- Liver Function Tests: These tests measure liver enzymes (ALT, AST), bilirubin, and albumin levels, helping to assess liver health and detect any worsening of the condition.
- Prothrombin Time (PT) and INR: These tests measure blood clotting, which can be impaired in liver disease.
Autoimmune Disorders
Conditions like rheumatoid arthritis and lupus require frequent blood tests to monitor disease activity and treatment efficacy:
- Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP): These markers indicate inflammation levels in the body, helping to assess disease activity.
- Autoantibody Tests: Specific tests, such as rheumatoid factor (RF) and antinuclear antibodies (ANA), help diagnose and monitor autoimmune conditions.
For individuals managing chronic conditions, regular blood tests are a cornerstone of effective disease management. They provide vital information that guides treatment decisions, monitors disease progression, and prevents complications. By keeping these crucial health markers in check, patients can lead healthier, more balanced lives, staying ahead of potential issues before they escalate into severe health crises.
Think of these tests as your personal health dashboard, giving you real-time updates and alerts to keep your health journey on the right track.
4. Optimising Athletic Performance

For athletes and fitness enthusiasts, blood tests are a game-changer, providing a wealth of information that can significantly enhance training, recovery, and overall performance. By tracking key biomarkers like hemoglobin, testosterone, and creatine kinase, athletes can tailor their regimens to achieve peak performance. Think of it as having your own personal sports science lab, giving you insights that go far beyond the surface level.
Hemoglobin: Hemoglobin is a protein in red blood cells responsible for carrying oxygen from the lungs to the rest of the body. For athletes, optimal hemoglobin levels are crucial because they directly influence oxygen delivery to muscles during exercise. Low hemoglobin levels can lead to anemia, characterized by fatigue and reduced endurance. Regular blood tests can help monitor hemoglobin and hematocrit levels, ensuring that any deficiencies are promptly addressed through dietary adjustments or supplementation, such as increasing iron intake.
Testosterone: Testosterone is a hormone that plays a vital role in muscle growth, strength, and recovery. It affects protein synthesis and the development of lean muscle mass. Both male and female athletes benefit from maintaining optimal testosterone levels. Blood tests can measure total and free testosterone, providing insights into hormonal balance. If levels are suboptimal, interventions can include lifestyle changes, dietary modifications, or medical treatments to restore balance, thereby enhancing muscle development and overall performance.
Creatine Kinase (CK): Creatine kinase is an enzyme found in the heart, brain, and skeletal muscles. Elevated CK levels in the blood often indicate muscle damage, which can occur after intense physical activity. Monitoring CK levels helps athletes understand the extent of muscle stress and recovery needs. High CK levels can prompt modifications in training intensity or frequency to prevent overtraining and reduce the risk of injury. This biomarker is particularly useful for tailoring recovery strategies, ensuring that muscles have adequate time to repair and grow stronger.
Lactate Threshold: Lactate threshold is the point during intense exercise at which lactate accumulates in the blood faster than it can be removed, leading to fatigue. Blood tests measuring lactate levels can help determine an athlete’s lactate threshold, which is crucial for designing effective training programs. By training just below this threshold, athletes can improve endurance and delay the onset of fatigue during competitions.
Cortisol: Cortisol, often referred to as the “stress hormone,” affects metabolism, immune function, and recovery. While short-term increases in cortisol can be beneficial for acute stress responses, chronically elevated cortisol levels can lead to muscle breakdown, fat accumulation, and impaired recovery. Blood tests measuring cortisol levels help athletes manage stress and optimize recovery protocols. Strategies to regulate cortisol include adequate sleep, proper nutrition, and stress management techniques such as mindfulness and relaxation exercises.
Electrolyte Balance: Electrolytes like sodium, potassium, and magnesium are vital for muscle function, hydration, and overall athletic performance. Blood tests can assess electrolyte levels, helping to prevent imbalances that could lead to muscle cramps, weakness, or more severe complications like hyponatremia or hyperkalemia. Ensuring optimal electrolyte balance through diet or supplements is essential for maintaining performance, especially in endurance sports.
Nutritional Status: Athletes have increased nutritional needs, and blood tests can evaluate levels of essential nutrients such as vitamin D, B vitamins, iron, and magnesium. Deficiencies in these nutrients can impair performance, increase injury risk, and prolong recovery times. By identifying and addressing these deficiencies, athletes can optimize their diet and supplementation to support energy production, muscle function, and overall health.
Hydration Status: Proper hydration is crucial for athletic performance. Blood tests can measure plasma osmolality and other markers to assess hydration status accurately. Dehydration can lead to decreased performance, heat-related illnesses, and longer recovery times. Monitoring hydration levels helps athletes maintain optimal fluid balance, ensuring peak performance during training and competition.
Inflammation Markers: Intense training can cause inflammation, which, if unmanaged, can lead to chronic injuries and decreased performance. Blood tests measuring markers like C-reactive protein (CRP) and interleukin-6 (IL-6) provide insights into the body’s inflammatory response. Managing inflammation through appropriate rest, anti-inflammatory foods, and recovery techniques is vital for long-term athletic success.
By leveraging the detailed insights provided by blood tests, athletes can make informed decisions about their training, nutrition, and recovery strategies. These tests serve as a scientific basis for optimizing performance, allowing for precise adjustments that can lead to significant improvements. Regular monitoring of these biomarkers ensures that athletes stay on the cutting edge of their performance potential, reducing the risk of injury and enhancing their ability to achieve their goals.
In summary, blood tests are not just a diagnostic tool; they are a strategic asset in the pursuit of athletic excellence. By understanding and utilizing this data, athletes can transform their approach to training and recovery, unlocking new levels of performance and endurance.
5. Hormonal Balance
Hormones rule our bodies like unseen emperors, orchestrating everything from metabolism to mood with precise coordination. Maintaining hormonal balance is crucial for overall health, and blood tests are a vital tool in assessing and managing hormone levels. By evaluating thyroid hormones, cortisol, and sex hormones, blood tests provide insights into various aspects of health, including energy levels, mood regulation, and metabolic function.
Thyroid Hormones: The thyroid gland produces hormones that regulate metabolism, energy production, and growth. Key thyroid hormones include:
Thyroxine (T4) and Triiodothyronine (T3): These hormones control the rate at which cells use energy and are essential for metabolic regulation. Blood tests measuring free T4 and T3 levels can diagnose conditions like hypothyroidism (underactive thyroid) and hyperthyroidism (overactive thyroid). Symptoms of hypothyroidism include fatigue, weight gain, and depression, while hyperthyroidism can cause weight loss, anxiety, and rapid heartbeat. Accurate diagnosis and treatment adjustments, including medication or lifestyle changes, can restore hormonal balance and improve overall well-being.
Thyroid-Stimulating Hormone (TSH): TSH, produced by the pituitary gland, regulates the production of T4 and T3. Elevated TSH levels typically indicate hypothyroidism, while low TSH levels suggest hyperthyroidism. Regular monitoring of TSH helps in fine-tuning thyroid treatment to maintain optimal hormone levels.
Cortisol: Cortisol, often referred to as the “stress hormone,” plays a critical role in the body’s stress response, metabolism, and immune function. Blood tests measuring cortisol levels can diagnose conditions like Cushing’s syndrome (high cortisol levels) and Addison’s disease (low cortisol levels).
- Diurnal Variation: Cortisol levels naturally fluctuate throughout the day, peaking in the morning and declining at night. Blood tests can assess this diurnal variation to identify abnormal patterns, which can indicate chronic stress, adrenal insufficiency, or other endocrine disorders. Managing cortisol levels through stress reduction techniques, adequate sleep, and, if necessary, medical interventions can significantly impact overall health and resilience.
Sex Hormones: Sex hormones, including estrogen, progesterone, and testosterone, influence a wide range of physiological processes from reproductive health to muscle mass and mood regulation.
Estrogen and Progesterone: These hormones are crucial for female reproductive health, regulating menstrual cycles, pregnancy, and menopause. Blood tests measuring estrogen (estradiol) and progesterone levels can diagnose conditions like polycystic ovary syndrome (PCOS), hormonal imbalances, and menopause-related issues. Symptoms of imbalances include irregular menstrual cycles, infertility, and mood swings. Hormone replacement therapy (HRT) or other treatments can help restore balance and alleviate symptoms.
Testosterone: Although testosterone is commonly associated with male health, it is also essential for women in smaller amounts. In men, testosterone is vital for muscle mass, bone density, libido, and overall energy levels. Blood tests measuring total and free testosterone can diagnose conditions like hypogonadism (low testosterone) and androgen excess in women. Symptoms of low testosterone include fatigue, decreased libido, and reduced muscle mass. Treatments include lifestyle changes, testosterone replacement therapy, and medications to balance hormone levels.
Insulin: Insulin, produced by the pancreas, regulates blood glucose levels by facilitating cellular glucose uptake. Insulin resistance, where cells become less responsive to insulin, can lead to type 2 diabetes.
- Fasting Insulin and Glucose Tolerance Tests: Blood tests measuring fasting insulin levels and glucose tolerance can diagnose insulin resistance and early stages of diabetes. Managing insulin levels through diet, exercise, and medication can prevent the progression to full-blown diabetes and improve metabolic health.
Growth Hormone: Growth hormone (GH), produced by the pituitary gland, stimulates growth, cell reproduction, and regeneration. Abnormal levels can indicate conditions like acromegaly (excess GH) or growth hormone deficiency.
- IGF-1 Levels: Blood tests measuring insulin-like growth factor 1 (IGF-1), a hormone stimulated by GH, can provide insights into GH activity. Maintaining appropriate GH levels is crucial for muscle growth, metabolic function, and overall physical development.
Conclusion: By assessing these critical hormones, blood tests offer a comprehensive view of your hormonal health. Understanding and managing hormonal balance is essential for maintaining energy levels, mood stability, and overall physiological function. Whether you’re dealing with thyroid imbalances, stress-related cortisol fluctuations, or reproductive health issues, regular monitoring through blood tests provides the data needed to make informed decisions about your health.
In essence, blood tests for hormonal balance are like having a finely tuned orchestra, ensuring each hormone plays its part harmoniously. This orchestration allows you to achieve optimal health, resilience, and well-being, navigating the complexities of modern life with grace and vitality.
6. Assessing Organ Function
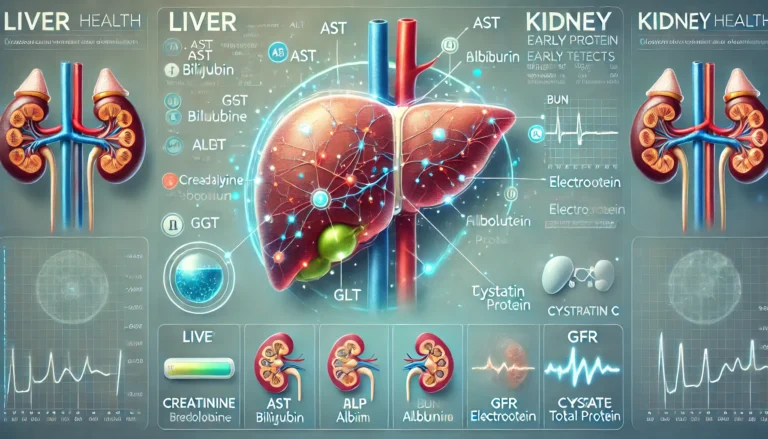
Your liver and kidneys are the unsung heroes of your body, working tirelessly to filter toxins, metabolise nutrients, and maintain overall homeostasis. Blood tests play a crucial role in assessing the health and functionality of these vital organs. By measuring specific enzymes and biomarkers, you can catch potential issues early, well before they escalate into serious problems.
Liver Function:
The liver performs over 500 functions, including detoxification, protein synthesis, and the production of biochemicals necessary for digestion. Blood tests can evaluate the liver’s performance by measuring various enzymes and proteins, each providing insight into different aspects of liver health.
Alanine Aminotransferase (ALT) and Aspartate Aminotransferase (AST): These enzymes are found in liver cells and are released into the bloodstream when liver cells are damaged. Elevated levels of ALT and AST can indicate liver inflammation or damage, which may be caused by conditions such as hepatitis, fatty liver disease, or cirrhosis.
Alkaline Phosphatase (ALP): This enzyme is present in the liver, bile ducts, and bone. High ALP levels can indicate bile duct obstruction, liver disease, or bone disorders. Monitoring ALP helps in diagnosing conditions like cholestasis or bone abnormalities.
Gamma-Glutamyl Transferase (GGT): GGT is an enzyme involved in the metabolism of glutathione and drug detoxification. Elevated GGT levels can be a marker of liver disease, bile duct problems, or chronic alcohol use. It is often measured alongside other liver enzymes to provide a comprehensive view of liver health.
Bilirubin: Bilirubin is a byproduct of the normal breakdown of red blood cells, processed by the liver and excreted in bile. High levels of bilirubin can lead to jaundice and may indicate liver dysfunction, bile duct blockage, or haemolytic anaemia. Total and direct bilirubin levels are measured to diagnose and monitor these conditions.
Albumin and Total Protein: The liver produces albumin, a protein that maintains blood oncotic pressure and transports hormones, vitamins, and drugs. Low levels of albumin and total protein can indicate liver disease, malnutrition, or kidney disease. These markers help assess the liver’s synthetic function.
Kidney Function:
The kidneys are responsible for filtering waste products, balancing electrolytes, and maintaining fluid balance. Blood tests for kidney function focus on markers that reflect how well the kidneys are filtering and excreting waste.
Creatinine: Creatinine is a waste product of muscle metabolism, filtered out of the blood by the kidneys. Elevated blood creatinine levels indicate impaired kidney function or chronic kidney disease (CKD). The glomerular filtration rate (GFR), calculated from creatinine levels, provides an estimate of kidney function and helps stage the severity of CKD.
Blood Urea Nitrogen (BUN): BUN measures the amount of nitrogen in the blood that comes from the waste product urea. Elevated BUN levels can indicate reduced kidney function, dehydration, or high protein intake. It is often used alongside creatinine to assess kidney health.
Electrolytes (Sodium, Potassium, and Chloride): The kidneys play a vital role in maintaining electrolyte balance. Blood tests measuring these electrolytes can detect imbalances caused by kidney dysfunction, dehydration, or certain medications. Abnormal levels of potassium, in particular, can have serious effects on heart function and require immediate attention.
Glomerular Filtration Rate (GFR): GFR is a measure of how well the kidneys are filtering blood. It is estimated using creatinine levels, age, sex, and body size. A low GFR indicates reduced kidney function and can help diagnose and monitor chronic kidney disease.
Cystatin C: Cystatin C is a protein that can be used as an alternative marker to creatinine for estimating GFR. It may provide a more accurate assessment of kidney function, especially in individuals with abnormal muscle mass or those who are elderly.
Early Detection and Intervention:
Regular blood tests to assess liver and kidney function are crucial for early detection and intervention. Many liver and kidney diseases are asymptomatic in the early stages, and routine blood work can identify problems before symptoms arise. Early diagnosis allows for timely treatment, which can slow disease progression, improve quality of life, and prevent complications.
For instance, detecting elevated liver enzymes might prompt further testing to identify the cause, leading to interventions such as lifestyle changes, medications, or procedures to treat underlying conditions. Similarly, identifying declining kidney function early can lead to dietary modifications, blood pressure control, and medications to protect kidney health and prevent end-stage renal disease.
Assessing liver and kidney function through blood tests is an essential aspect of proactive healthcare. These tests provide valuable insights into the performance and health of these vital organs, enabling early detection and management of potential issues. By regularly monitoring liver and kidney markers, you can ensure that these organs continue to function effectively, supporting overall health and well-being.
Think of blood tests as the maintenance checks that keep your body’s engine running smoothly. Just as you wouldn’t ignore a warning light on your car’s dashboard, paying attention to your liver and kidney health can prevent small issues from turning into major problems, ensuring a healthier future.
7. Evaluating Heart Health
With cardiovascular diseases being a leading cause of death globally, keeping tabs on your heart health is crucial. Blood tests offer an essential window into your cardiovascular health by measuring cholesterol levels, triglycerides, and other key markers. These tests provide a clear picture of your heart’s current status and help guide interventions to reduce the risk of heart disease.
Cholesterol Levels:
Cholesterol is a lipid essential for building cell membranes and producing hormones, but imbalances can lead to cardiovascular problems. Blood tests for cholesterol typically include:
- Total Cholesterol: This measures the overall amount of cholesterol in your blood. While total cholesterol gives a general sense of risk, it’s the breakdown into LDL and HDL that provides more actionable insights.
- Low-Density Lipoprotein (LDL): Often referred to as “bad cholesterol,” LDL can accumulate in the walls of your arteries, forming plaques that narrow and harden arteries, a condition known as atherosclerosis. Elevated LDL levels increase the risk of heart attack and stroke.
- High-Density Lipoprotein (HDL): Known as “good cholesterol,” HDL helps remove excess cholesterol from the bloodstream and transport it to the liver for excretion. Higher HDL levels are generally associated with a lower risk of heart disease.
- Non-HDL Cholesterol: This includes all cholesterol particles that aren’t HDL, providing a comprehensive risk assessment. Non-HDL cholesterol is considered a better predictor of heart disease risk than LDL alone.
Triglycerides:
Triglycerides are another type of fat found in the blood. After eating, your body converts excess calories into triglycerides, which are stored in fat cells. Elevated triglyceride levels can increase the risk of coronary artery disease, especially when combined with high LDL or low HDL levels. Blood tests measuring triglyceride levels help assess the risk of metabolic syndrome, a cluster of conditions that increase heart disease, stroke, and diabetes risk.
C-Reactive Protein (CRP):
CRP is a marker of inflammation in the body. Chronic inflammation plays a significant role in the development of atherosclerosis. High-sensitivity CRP (hs-CRP) tests can detect low levels of inflammation, helping to predict the risk of cardiovascular events. Elevated hs-CRP levels can indicate increased risk, prompting lifestyle changes or medical interventions to reduce inflammation and improve heart health.
Lipoprotein(a):
Lipoprotein(a), or Lp(a), is a type of LDL particle with an additional protein called apolipoprotein(a). High levels of Lp(a) are a genetic risk factor for atherosclerosis and cardiovascular disease. Blood tests measuring Lp(a) can identify individuals at higher risk, even if their other cholesterol levels are within normal ranges. While Lp(a) levels are largely determined by genetics and less responsive to lifestyle changes, knowing your Lp(a) status can guide more aggressive management of other cardiovascular risk factors.
Apolipoprotein B (ApoB):
ApoB is a primary protein component of atherogenic lipoproteins, including LDL, VLDL, and Lp(a). Measuring ApoB provides a direct count of these particles, offering a more precise assessment of cardiovascular risk than LDL cholesterol alone. Elevated ApoB levels indicate a higher number of atherogenic particles, which can accelerate plaque formation and increase the risk of heart disease.
Natriuretic Peptides:
B-type natriuretic peptide (BNP) and N-terminal pro-BNP (NT-proBNP) are hormones produced by the heart in response to stretching caused by increased blood volume. Elevated levels of these peptides indicate heart failure and can help diagnose the severity of the condition. Blood tests measuring BNP or NT-proBNP are crucial for managing heart failure, guiding treatment decisions, and monitoring disease progression.
Glucose and Haemoglobin A1c (HbA1c):
High blood sugar levels can damage blood vessels and contribute to the development of cardiovascular disease. Blood tests measuring fasting glucose and HbA1c levels help assess the risk of diabetes, a significant risk factor for heart disease. Managing blood sugar levels through diet, exercise, and medication can reduce cardiovascular risk and improve overall heart health.
Evaluating heart health through blood tests is an integral part of preventative medicine. These tests provide a comprehensive view of the various factors influencing cardiovascular health, from lipid levels and inflammation to genetic risk markers. By regularly monitoring these biomarkers, you can take proactive steps to reduce your risk of heart disease, whether through lifestyle modifications, dietary changes, or medical treatments.
Think of blood tests as a diagnostic tool that helps you stay ahead of potential heart problems. With the right information, you can make informed decisions to protect your heart, ensuring it remains strong and healthy for years to come.
8. Early Detection Of Disease
Blood tests are a cornerstone of modern medicine, providing invaluable insights that can lead to the early detection of a wide range of diseases, including cancer, autoimmune disorders, and infections. Early detection is crucial as it allows for timely intervention, which can be lifesaving. By identifying disease markers before symptoms manifest, blood tests offer a proactive approach to health management, significantly improving outcomes.
Cancer Detection
Blood tests can identify specific markers associated with various types of cancer, aiding in early diagnosis and monitoring. These markers include:
Tumor Markers: Substances produced by cancer cells or by the body in response to cancer. Examples include Prostate-Specific Antigen (PSA) for prostate cancer, CA-125 for ovarian cancer, and Carcinoembryonic Antigen (CEA) for colorectal cancer. Elevated levels of these markers can indicate the presence of cancer, prompting further diagnostic investigations.
Circulating Tumor Cells (CTCs): These cells are shed by tumors into the bloodstream. Detecting CTCs through blood tests can provide early indications of metastasis and help in monitoring treatment response.
Liquid Biopsies: Advanced blood tests that analyze fragments of tumor DNA circulating in the blood. Liquid biopsies can detect genetic mutations and alterations associated with cancer, enabling early diagnosis, monitoring of treatment efficacy, and detection of recurrence.
Autoimmune Disorders
Autoimmune disorders occur when the immune system mistakenly attacks the body’s own tissues. Blood tests can detect specific autoantibodies and markers of inflammation, helping to diagnose and manage these conditions.
Antinuclear Antibodies (ANA): These antibodies target the cell nucleus and are commonly found in autoimmune diseases like systemic lupus erythematosus (SLE). A positive ANA test can indicate the presence of an autoimmune disorder, necessitating further testing for specific antibodies.
Rheumatoid Factor (RF) and Anti-Cyclic Citrullinated Peptide (Anti-CCP): These markers are associated with rheumatoid arthritis. Elevated levels of RF and Anti-CCP antibodies can confirm the diagnosis and guide treatment plans.
Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP): These markers measure inflammation levels in the body. Elevated ESR and CRP can indicate active autoimmune disease and help monitor the effectiveness of treatment.
Infections
Blood tests are essential for diagnosing infections, identifying the causative agents, and guiding appropriate treatment.
Complete Blood Count (CBC): A CBC can detect changes in white blood cell counts, indicating the presence of infection. Elevated levels of neutrophils suggest bacterial infection, while increased lymphocytes may indicate viral infection.
Blood Cultures: These tests identify bacteria or fungi present in the bloodstream, crucial for diagnosing septicemia and determining the most effective antibiotic or antifungal treatment.
Serologic Tests: These tests detect antibodies or antigens associated with specific infections. For example, the presence of HIV antibodies confirms HIV infection, while Hepatitis B surface antigen (HBsAg) indicates an active Hepatitis B infection.
Chronic Diseases
Blood tests can also detect early signs of chronic diseases, allowing for timely intervention to prevent progression.
Diabetes: Blood glucose tests and Hemoglobin A1c (HbA1c) measurements can identify prediabetes and diabetes before severe symptoms develop. Early management can prevent complications such as neuropathy, retinopathy, and cardiovascular disease.
Cardiovascular Disease: Elevated levels of cholesterol, triglycerides, and markers of inflammation like CRP can indicate an increased risk of heart disease. Early detection allows for lifestyle changes and treatments to reduce risk.
Genetic Disorders
Genetic screening through blood tests can identify carriers of genetic disorders and diagnose inherited conditions.
BRCA1 and BRCA2 Mutations: These genetic mutations significantly increase the risk of breast and ovarian cancers. Identifying carriers can prompt preventive measures, such as increased surveillance or prophylactic surgeries.
Cystic Fibrosis (CF) Screening: Blood tests can detect mutations in the CFTR gene, diagnosing cystic fibrosis in newborns and guiding early intervention to manage symptoms and improve quality of life.
Blood tests are a powerful tool for the early detection of diseases, offering a proactive approach to healthcare. By identifying disease markers before symptoms appear, these tests enable early intervention, which can be lifesaving. Whether it’s detecting cancer, autoimmune disorders, infections, or chronic diseases, regular blood testing provides critical insights that guide timely and effective treatment.
Think of blood tests as your body’s early warning system, alerting you to potential health issues long before they become serious. With early detection, you can take control of your health, ensuring better outcomes and a healthier future.
9. Diet Personalisation

Ever wondered if you’re eating the right foods? Blood tests can reveal how your body reacts to different nutrients, helping you personalize your diet for optimal health and performance. By understanding your unique biochemical makeup, you can make informed dietary choices that enhance your overall well-being, support your fitness goals, and prevent chronic diseases.
Nutrient Deficiencies
Blood tests can identify deficiencies in essential vitamins and minerals that are critical for various bodily functions.
Iron: Iron is crucial for oxygen transport and energy production. Blood tests measuring serum ferritin and hemoglobin levels can diagnose iron deficiency anemia, which can cause fatigue and decreased physical performance. Addressing this deficiency through dietary changes or supplementation can improve energy levels and cognitive function.
Vitamin D: Vitamin D plays a vital role in bone health, immune function, and mood regulation. Blood tests measuring 25-hydroxyvitamin D [25(OH)D] levels can determine if you are deficient. Supplementing with vitamin D or increasing sun exposure can enhance bone density, reduce the risk of fractures, and improve overall health.
Vitamin B12: Essential for nerve function and red blood cell production, vitamin B12 deficiency can lead to anemia, fatigue, and neurological issues. Blood tests measuring serum B12 and methylmalonic acid (MMA) levels can identify a deficiency. Dietary adjustments or B12 supplementation can mitigate these symptoms and support neurological health.
Magnesium: Magnesium is involved in over 300 biochemical reactions, including muscle function, energy production, and blood glucose control. Blood tests measuring serum magnesium levels can detect deficiencies that may cause muscle cramps, hypertension, and metabolic disorders. Correcting low magnesium levels through diet or supplements can improve muscle performance and cardiovascular health.
Food Sensitivities and Allergies
Food sensitivities and allergies can significantly impact your health and quality of life. Blood tests can help identify these issues.
- IgE and IgG Antibodies: Blood tests measuring IgE antibodies can diagnose immediate allergic reactions to foods like peanuts, shellfish, and dairy. IgG antibody tests can identify delayed food sensitivities, which may cause symptoms such as bloating, headaches, and joint pain. Eliminating or reducing these foods from your diet can alleviate symptoms and improve overall well-being.
Metabolic Health
Understanding your metabolic health can guide dietary choices that support weight management, energy levels, and disease prevention.
Blood Glucose and Insulin Levels: Blood tests measuring fasting blood glucose and insulin levels can assess your risk of developing insulin resistance and type 2 diabetes. Analyzing Hemoglobin A1c (HbA1c) levels provides insights into long-term blood sugar control. Tailoring your diet to include low-glycemic index foods and reducing sugar intake can help manage blood glucose levels and prevent diabetes.
Lipid Profile: A comprehensive lipid profile measures total cholesterol, LDL, HDL, and triglycerides, providing a snapshot of your cardiovascular health. High levels of LDL and triglycerides or low HDL levels can increase the risk of heart disease. Adjusting your diet to include heart-healthy fats, fiber-rich foods, and reducing saturated fat intake can improve your lipid profile and reduce cardiovascular risk.
Macronutrient Ratios
Blood tests can help determine the optimal macronutrient ratios for your body, enhancing athletic performance and supporting specific health goals.
Amino Acids Profile: Amino acids are the building blocks of proteins, essential for muscle repair, immune function, and neurotransmitter production. Blood tests measuring amino acid levels can identify imbalances that may affect muscle recovery and mental health. Ensuring adequate protein intake from diverse sources can optimize muscle growth and cognitive function.
Fatty Acids Profile: Omega-3 and omega-6 fatty acids are crucial for inflammatory responses, brain function, and cardiovascular health. Blood tests measuring these fatty acids can help balance your intake of omega-3-rich foods like fish, flaxseeds, and walnuts, while reducing omega-6-rich processed foods to promote anti-inflammatory effects and improve heart health.
Personalised Diet Plans
Blood tests provide the data needed to create personalised diet plans tailored to your unique needs.
Genetic Testing: Nutrigenomics is the study of how genes and nutrients interact. Genetic testing can reveal specific genetic variations that influence nutrient metabolism, food intolerances, and susceptibility to certain diseases. By understanding your genetic profile, you can make dietary choices that align with your genetic predispositions, optimizing your health and preventing chronic conditions.
Micronutrient Testing: Comprehensive micronutrient tests measure a wide range of vitamins, minerals, antioxidants, and other nutrients in your blood. Identifying deficiencies or imbalances allows for targeted dietary interventions, ensuring you receive the right nutrients in the right amounts.
Blood tests are a powerful tool for tailoring your diet to meet your specific health needs and goals. By providing detailed insights into nutrient deficiencies, food sensitivities, metabolic health, and genetic predispositions, these tests enable you to make informed dietary choices that enhance your overall well-being.
Think of blood tests as the ultimate personalised nutrition guide, offering a roadmap to better health through tailored dietary adjustments. By aligning your diet with your unique biochemical makeup, you can achieve optimal health, improve athletic performance, and reduce the risk of chronic diseases.
10. Managing Stress
High-stress levels can wreak havoc on your health, impacting everything from your cardiovascular system to your mental well-being. Blood tests measuring cortisol levels provide a comprehensive view of your stress profile, allowing you to manage stress more effectively through lifestyle changes or medical interventions. Understanding how stress affects your body can lead to significant improvements in overall health and quality of life.
Cortisol: The Stress Hormone
Cortisol is often referred to as the “stress hormone” because it plays a key role in the body’s response to stress. Produced by the adrenal glands, cortisol helps regulate metabolism, immune response, and the body’s use of fats, proteins, and carbohydrates. It also influences memory formation, salt and water balance, and blood pressure.
Diurnal Variation: Cortisol levels follow a diurnal rhythm, peaking in the early morning and gradually declining throughout the day. Blood tests can measure cortisol at different times to assess whether this pattern is maintained. Abnormal cortisol patterns can indicate chronic stress, adrenal fatigue, or disorders such as Cushing’s syndrome (excess cortisol) or Addison’s disease (insufficient cortisol).
Salivary Cortisol: Salivary cortisol tests are less invasive and can be done at home, providing a convenient way to measure cortisol levels at multiple points throughout the day. This method helps capture the natural fluctuations in cortisol levels, offering a more accurate picture of your stress response.
Impact of Chronic Stress
Chronic stress can lead to prolonged high cortisol levels, which have numerous negative effects on the body:
Cardiovascular Health: Elevated cortisol levels increase blood pressure and heart rate, contributing to hypertension and increasing the risk of cardiovascular diseases. Chronic stress can also lead to the accumulation of visceral fat, further heightening cardiovascular risk.
Immune System: High cortisol levels suppress the immune system, making the body more susceptible to infections and slowing down the healing process. Chronic stress can also exacerbate autoimmune conditions and increase inflammation.
Metabolism and Weight: Cortisol influences appetite and can lead to cravings for high-calorie foods. Chronic stress is associated with weight gain, particularly around the abdomen, and can contribute to metabolic syndrome, a cluster of conditions that increase the risk of heart disease, stroke, and diabetes.
Mental Health: Prolonged exposure to high cortisol levels affects brain function, leading to memory impairment, reduced cognitive performance, and an increased risk of anxiety and depression.
Managing Stress Through Lifestyle Changes
Understanding your cortisol levels through blood tests can guide effective stress management strategies:
Exercise: Regular physical activity reduces cortisol levels and helps manage stress. Aerobic exercises like walking, running, and swimming are particularly effective. Strength training and yoga can also improve mood and reduce stress.
Nutrition: A balanced diet rich in whole foods can help regulate cortisol levels. Foods high in omega-3 fatty acids, like salmon and walnuts, have anti-inflammatory properties that can mitigate the effects of stress. Reducing caffeine and sugar intake can also help maintain stable cortisol levels.
Sleep: Quality sleep is crucial for maintaining healthy cortisol levels. Aim for 7-9 hours of sleep per night and establish a regular sleep routine. Avoiding screens before bed and creating a relaxing bedtime environment can improve sleep quality.
Mindfulness and Relaxation Techniques: Practices like mindfulness meditation, deep breathing, and progressive muscle relaxation can lower cortisol levels and promote a sense of calm. These techniques help shift the body from a stress response to a relaxation response, reducing overall stress levels.
Social Support: Building strong social connections and seeking support from friends, family, or support groups can buffer the effects of stress. Talking about your stressors with others can provide emotional relief and practical solutions.
Medical Interventions
In cases where lifestyle changes are insufficient, medical interventions may be necessary to manage cortisol levels:
Cognitive Behavioural Therapy (CBT): CBT is a type of psychotherapy that helps individuals identify and change negative thought patterns and behaviours that contribute to stress. It is effective in treating anxiety, depression, and stress-related disorders.
Medications: In some cases, medications such as antidepressants or anti-anxiety drugs may be prescribed to help manage symptoms of chronic stress. These medications should be used under the guidance of a healthcare professional.
Adrenal Support: For those with adrenal insufficiency or adrenal fatigue, specific treatments may be required to support adrenal function. This can include hormone replacement therapy or supplements designed to support adrenal health.
Managing stress is essential for maintaining overall health and well-being. Blood tests measuring cortisol levels provide valuable insights into your stress profile, allowing for targeted interventions to reduce stress and its harmful effects. Whether through lifestyle changes, mindfulness practices, or medical treatments, understanding and managing your stress can lead to significant improvements in your physical and mental health.
Think of cortisol tests as a diagnostic tool that helps you decode your body’s stress signals. By understanding your stress profile, you can take proactive steps to manage stress effectively, ensuring a healthier and more balanced life.
11. Tracking Inflammation

Chronic inflammation is a silent threat that can significantly impact your health, contributing to the development of various diseases, including heart disease, arthritis, diabetes, and even cancer. Blood tests that measure specific markers can provide a detailed picture of your inflammation levels, enabling early detection and intervention to mitigate these risks.
Understanding Inflammation
Inflammation is a natural response of the immune system to injury or infection. Acute inflammation, such as redness and swelling from a cut, is a protective mechanism that helps the body heal. However, chronic inflammation is a prolonged and often subtle process that can damage tissues and organs over time, leading to serious health conditions.
Key Inflammatory Markers:
Blood tests can measure several markers that indicate the presence and severity of inflammation in the body:
C-Reactive Protein (CRP): CRP is produced by the liver in response to inflammation. High-sensitivity CRP (hs-CRP) tests can detect low levels of CRP in the blood, providing a sensitive measure of chronic inflammation. Elevated CRP levels are associated with an increased risk of cardiovascular diseases, such as heart attack and stroke, as well as other chronic conditions.
Erythrocyte Sedimentation Rate (ESR): ESR measures the rate at which red blood cells settle at the bottom of a test tube. A faster rate indicates the presence of inflammation. While ESR is a less specific marker than CRP, it can be useful in diagnosing and monitoring inflammatory diseases such as rheumatoid arthritis and lupus.
Interleukins (IL-6, IL-1β): Interleukins are a group of cytokines (proteins) that play a crucial role in the immune response. IL-6 and IL-1β are pro-inflammatory cytokines that can be measured to assess the level of inflammation. Elevated levels of these cytokines are associated with chronic inflammatory conditions and autoimmune diseases.
Tumor Necrosis Factor-alpha (TNF-α): TNF-α is another cytokine involved in systemic inflammation. High levels of TNF-α are linked to conditions such as inflammatory bowel disease, rheumatoid arthritis, and psoriasis. Measuring TNF-α can help in diagnosing and monitoring these conditions.
Impact of Chronic Inflammation
Chronic inflammation is linked to a wide range of diseases, making it a critical factor to monitor:
Cardiovascular Disease: Chronic inflammation contributes to the development of atherosclerosis, where plaque builds up in the arteries, leading to heart attacks and strokes. Elevated CRP levels are a strong predictor of cardiovascular events.
Arthritis: Inflammatory markers like CRP and ESR are elevated in conditions such as rheumatoid arthritis and osteoarthritis. Monitoring these markers helps assess disease activity and guide treatment decisions to reduce joint damage and pain.
Diabetes: Inflammation plays a role in the development of insulin resistance, a precursor to type 2 diabetes. High levels of inflammatory markers are associated with an increased risk of developing diabetes and its complications.
Cancer: Chronic inflammation can promote tumor growth and progression. Conditions like chronic inflammatory bowel disease are linked to a higher risk of colorectal cancer. Monitoring inflammatory markers can help in early detection and management of cancer risk.
Managing Inflammation
Understanding your inflammation levels through blood tests allows for targeted strategies to manage and reduce chronic inflammation:
Anti-inflammatory Diet: A diet rich in anti-inflammatory foods can help reduce inflammation. Incorporate plenty of fruits, vegetables, whole grains, fatty fish, nuts, and seeds into your diet. Foods rich in omega-3 fatty acids, such as salmon and flaxseeds, have particularly potent anti-inflammatory effects. Avoiding processed foods, sugary drinks, and trans fats is also crucial.
Regular Exercise: Physical activity helps reduce inflammation and improve overall health. Aim for at least 150 minutes of moderate-intensity exercise or 75 minutes of vigorous-intensity exercise per week. Activities like walking, swimming, and yoga can be particularly beneficial.
Stress Management: Chronic stress can exacerbate inflammation. Techniques such as mindfulness meditation, deep breathing exercises, and yoga can help manage stress levels and reduce inflammation.
Adequate Sleep: Poor sleep is associated with increased inflammation. Aim for 7-9 hours of quality sleep per night. Establishing a regular sleep routine and creating a restful environment can improve sleep quality.
Smoking Cessation: Smoking is a significant contributor to chronic inflammation. Quitting smoking can greatly reduce inflammation levels and improve overall health.
Medications and Supplements: In some cases, medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroids may be prescribed to reduce inflammation. Supplements like omega-3 fatty acids, turmeric (curcumin), and green tea extract can also have anti-inflammatory effects. Always consult with a healthcare provider before starting any new medication or supplement.
Tracking inflammation through blood tests is a proactive step in maintaining and improving your health. By measuring markers such as CRP, ESR, interleukins, and TNF-α, you can gain valuable insights into your body’s inflammatory status and take steps to mitigate chronic inflammation.
Think of these blood tests as an early warning system, alerting you to potential health risks before they become serious. With this information, you can make informed lifestyle and dietary changes, manage stress, and, if necessary, seek medical interventions to keep chronic inflammation in check. By doing so, you can reduce your risk of developing inflammation-related diseases and enjoy a healthier, more vibrant life.
12. Monitoring Blood Sugars
Monitoring blood glucose levels is a fundamental aspect of managing overall health, particularly for those at risk of diabetes. Blood tests provide critical insights into your blood sugar patterns, enabling you to make informed decisions about diet, exercise, and medication to maintain optimal health. Understanding these patterns is essential for preventing complications associated with diabetes and ensuring long-term well-being.
Understanding Blood Glucose
Blood glucose, or blood sugar, is the primary source of energy for the body’s cells. It is derived from the food we eat and is regulated by the hormone insulin, produced by the pancreas. Maintaining stable blood glucose levels is crucial for metabolic health and preventing the onset of diabetes.
Key Blood Glucose Tests:
Several blood tests can measure blood glucose levels and provide insights into your risk of developing diabetes or how well your diabetes is being managed:
Fasting Blood Glucose (FBG): This test measures blood sugar levels after an overnight fast. Normal fasting blood glucose levels are typically between 70 and 99 mg/dL. Levels between 100 and 125 mg/dL indicate prediabetes, and levels of 126 mg/dL or higher suggest diabetes. Fasting blood glucose tests are a standard method for diagnosing diabetes and prediabetes.
Hemoglobin A1c (HbA1c): The HbA1c test measures the average blood glucose levels over the past two to three months by assessing the amount of glucose attached to hemoglobin in red blood cells. An HbA1c level below 5.7% is considered normal, 5.7% to 6.4% indicates prediabetes, and 6.5% or higher suggests diabetes. The HbA1c test provides a long-term view of blood sugar control, making it a valuable tool for diabetes management.
Oral Glucose Tolerance Test (OGTT): This test measures blood glucose levels before and after consuming a glucose-rich drink. Blood sugar levels are measured at fasting, then one and two hours after drinking the solution. The OGTT is particularly useful for diagnosing gestational diabetes and prediabetes. A two-hour blood glucose level of 140 to 199 mg/dL indicates prediabetes, while a level of 200 mg/dL or higher confirms diabetes.
Random Blood Glucose Test: This test measures blood sugar levels at any time of the day, regardless of when you last ate. It is often used in conjunction with other tests to diagnose diabetes. A random blood glucose level of 200 mg/dL or higher suggests diabetes, especially if accompanied by symptoms such as increased thirst, frequent urination, and unexplained weight loss.
Impact of High Blood Sugar
Consistently high blood glucose levels can lead to a range of health complications, including:
Cardiovascular Disease: High blood sugar can damage blood vessels and nerves, increasing the risk of heart disease and stroke. Diabetes is a significant risk factor for cardiovascular conditions.
Neuropathy: Excess glucose can damage nerves, leading to diabetic neuropathy. Symptoms include pain, tingling, and loss of sensation in the extremities, which can lead to severe complications like foot ulcers and amputations.
Retinopathy: High blood sugar levels can damage the blood vessels in the retina, leading to diabetic retinopathy, which can cause vision loss and blindness if untreated.
Kidney Disease: Diabetes can damage the kidneys’ filtering system, leading to diabetic nephropathy. This condition can progress to kidney failure, necessitating dialysis or a kidney transplant.
Infections: High blood glucose levels can impair the immune system, making individuals more susceptible to infections, including skin infections and urinary tract infections.
Managing Blood Glucose Levels
Monitoring blood glucose levels through regular blood tests allows for effective management strategies to keep blood sugar within a healthy range:
Diet: Adopting a balanced diet that focuses on whole foods, low in refined sugars and carbohydrates, can help maintain stable blood glucose levels. Emphasize fiber-rich vegetables, lean proteins, and healthy fats. Monitoring carbohydrate intake and understanding the glycemic index of foods can aid in better blood sugar control.
Exercise: Regular physical activity helps improve insulin sensitivity and lowers blood sugar levels. Aim for at least 150 minutes of moderate-intensity exercise per week, such as walking, cycling, or swimming. Strength training exercises are also beneficial for improving glucose metabolism.
Medication: For individuals with diabetes, medication may be necessary to manage blood sugar levels. This can include oral medications like metformin or insulin therapy. Regular blood tests help adjust medication dosages to achieve optimal glucose control.
Continuous Glucose Monitoring (CGM): CGM devices provide real-time data on blood glucose levels throughout the day and night, offering a comprehensive view of glucose patterns. This technology allows for more precise adjustments in diet, exercise, and medication, improving overall diabetes management.
Lifestyle Modifications: Stress management techniques, adequate sleep, and avoiding smoking and excessive alcohol consumption can also positively impact blood glucose levels and overall health.
Keeping an eye on blood sugar levels through regular blood tests is essential for preventing and managing diabetes. These tests provide crucial insights into your blood glucose patterns, enabling better management through diet, exercise, and medication if needed. By monitoring and maintaining healthy blood sugar levels, you can reduce the risk of diabetes-related complications and enjoy a healthier, more active life.
Think of these blood tests as your guide to navigating the complex world of blood sugar management. With the right information, you can make informed choices that support your long-term health and well-being, ensuring you stay on the path to a healthier future.
The Blood Testing Procedure

Getting a blood test is a straightforward and essential step in assessing and maintaining your health. The process involves several key steps, each designed to ensure accurate and reliable results that can provide invaluable insights into your body’s functioning. Here’s a detailed look at what happens during the blood testing procedure.
Step 1: Preparation
Before the blood draw, there may be specific instructions to follow, depending on the type of test being performed. For example:
- Fasting: Some tests, like fasting blood glucose or lipid profiles, require fasting for 8-12 hours before the blood draw. This means you should not eat or drink anything except water.
- Medication: You may be advised to continue or temporarily stop certain medications that could affect the test results. Always follow your healthcare provider’s instructions regarding medication.
Step 2: Blood Draw
The actual process of drawing blood, also known as phlebotomy, is typically quick and minimally uncomfortable:
- Location: Blood is usually drawn from a vein in your arm. The median cubital vein, located in the bend of your elbow, is a common site because it is close to the surface and generally easy to access.
- Preparation: The healthcare professional will clean the puncture site with an antiseptic to prevent infection. An elastic band, or tourniquet, is placed around your upper arm to fill the veins with blood, making them easier to see and access.
- Drawing Blood: A sterile needle is inserted into the vein, and a small amount of blood is collected into one or more vials or tubes. You might feel a brief sting or pinch as the needle is inserted.
- Post-Draw Care: After the blood is drawn, the needle is removed, and pressure is applied to the site with a cotton ball or gauze to stop the bleeding. A bandage is then placed over the site.
Step 3: Handling and Transport
Once the blood is drawn, it must be properly handled and transported to the laboratory for analysis:
- Labelling: Each vial is carefully labeled with your details, including your name, date of birth, and the specific tests ordered, to ensure accurate tracking and results.
- Storage: Depending on the tests, some blood samples need to be refrigerated, kept at room temperature, or processed immediately. The lab technician will handle the samples according to specific protocols to preserve their integrity.
- Transport: Samples are transported to the laboratory under controlled conditions to prevent degradation. Proper handling is crucial for maintaining sample quality and ensuring accurate results.
Step 4: Laboratory Analysis
At the laboratory, sophisticated techniques and equipment are used to analyse the blood samples. The process includes:
- Preparation: Upon arrival at the lab, samples are logged and prepared for analysis. Some tests require centrifugation, where the blood is spun at high speeds to separate its components, such as plasma, serum, or cells.
- Automated Analysis: Many blood tests are performed using automated analysers. These machines are capable of performing a large number of tests quickly and accurately, measuring a wide range of biomarkers such as glucose, cholesterol, electrolytes, enzymes, and hormones.
- Specialised Testing: Some tests require more specialised techniques, such as polymerase chain reaction (PCR) for detecting genetic material, immunoassays for hormone levels, or mass spectrometry for detailed metabolic profiling.
Step 5: Results and Interpretation
Once the analysis is complete, the results are compiled and interpreted:
- Report Generation: The lab generates a report detailing the levels of various biomarkers tested. These results are compared against reference ranges to determine if they fall within normal limits.
- Clinical Interpretation: Your healthcare provider will review the results, considering your medical history, symptoms, and other relevant factors. They will interpret the findings to diagnose conditions, assess health status, or monitor the effectiveness of treatments.
- Follow-Up: Based on the results, your healthcare provider may recommend further testing, lifestyle modifications, or specific treatments. They will discuss the findings with you and answer any questions you may have.
Common Blood Tests and Biomarkers
Understanding the specific tests and biomarkers can enhance your knowledge of what your blood test results mean:
- Complete Blood Count (CBC): Measures red blood cells, white blood cells, haemoglobin, haematocrit, and platelets. It can detect anaemia, infections, and other haematologic conditions.
- Basic Metabolic Panel (BMP): Includes tests for glucose, calcium, and electrolytes (sodium, potassium, carbon dioxide, and chloride). It assesses metabolic function and kidney health.
- Lipid Panel: Measures total cholesterol, LDL (bad) cholesterol, HDL (good) cholesterol, and triglycerides. It evaluates cardiovascular risk.
- Liver Function Tests (LFTs): Includes ALT, AST, alkaline phosphatase (ALP), bilirubin, and albumin. It assesses liver health and function.
- Thyroid Function Tests: Measures TSH, free T4, and free T3. It evaluates thyroid gland function and detects hypo- or hyperthyroidism.
- Haemoglobin A1c (HbA1c): Provides an average blood glucose level over the past 2-3 months. It is used to diagnose and monitor diabetes.
The blood testing procedure, though seemingly simple, involves a series of meticulous steps to ensure accuracy and reliability. From the initial blood draw to the detailed analysis in the laboratory, each phase is crucial for providing meaningful insights into your health. By understanding the process and the significance of various biomarkers, you can better appreciate the value of regular blood tests in maintaining and improving your health.
Think of blood tests as a comprehensive health check-up that provides a wealth of information about your body’s inner workings. With the detailed insights gained from these tests, you and your healthcare provider can make informed decisions to promote optimal health and well-being.
How Blood is Analysed
Once your blood sample reaches the laboratory, it undergoes a series of meticulous tests to evaluate its various components. This process combines advanced automated technologies with the expertise of skilled technicians to ensure accurate and reliable results. The analysis of your blood can reveal detailed information about your health, from the number of red and white blood cells to the levels of enzymes, hormones, and nutrients. Here’s an in-depth look at how blood is analysed in the lab.
Sample Preparation
Upon arrival at the laboratory, the blood sample is logged and prepared for analysis:
- Centrifugation: Many blood tests require separating the blood into its components: red blood cells, white blood cells, platelets, and plasma or serum. This is typically done using a centrifuge, which spins the blood sample at high speeds to separate the heavier cells from the lighter plasma/serum.
- Aliquoting: Depending on the tests ordered, the separated components may be divided into smaller aliquots for different types of analyses. Each aliquot is carefully labeled and handled according to specific protocols.
Automated Analysis
Modern laboratories rely heavily on automated analysers for efficient and precise testing. These machines can perform a wide range of tests rapidly and with high accuracy:
- Haematology Analysers: These machines are used to perform complete blood counts (CBC). They measure and count the different types of cells in the blood, including red blood cells, white blood cells, and platelets. Haematology analysers can also measure haemoglobin concentration and calculate haematocrit levels, providing essential information about oxygen transport and blood volume.
- Clinical Chemistry Analysers: These analysers measure the levels of various chemicals and substances in the blood, such as glucose, cholesterol, electrolytes, and enzymes. They use techniques like photometry, which measures the intensity of light absorbed by the sample, to quantify these substances accurately.
- Immunoassay Analysers: These machines detect and measure specific proteins, hormones, and antibodies in the blood using immunological techniques. Immunoassays are used for a wide range of tests, including hormone levels (like thyroid hormones and reproductive hormones), markers of infection (such as HIV or hepatitis), and tumour markers.
Specialised Techniques:
Some blood tests require more specialised techniques to analyse complex biomarkers or detect minute quantities of substances:
- Mass Spectrometry: This technique is used to identify and quantify molecules based on their mass-to-charge ratio. Mass spectrometry is particularly useful for detecting and measuring metabolites, drugs, and hormones in the blood. It provides high sensitivity and specificity, making it ideal for detailed metabolic profiling and pharmacokinetic studies.
- Polymerase Chain Reaction (PCR): PCR is used to amplify and detect specific genetic material in the blood. This technique is essential for diagnosing genetic disorders, detecting viral infections (such as COVID-19), and monitoring certain types of cancer. PCR can identify even small amounts of DNA or RNA, providing rapid and accurate results.
- Flow Cytometry: This technique analyses the physical and chemical characteristics of cells in the blood. Flow cytometry is used to diagnose and monitor blood cancers (such as leukaemia and lymphoma), assess immune function, and detect rare cell populations. It involves passing the cells through a laser beam and measuring the light scattered and emitted by fluorescently labeled antibodies bound to specific cell markers.
Quality Control and Validation
Ensuring the accuracy and reliability of blood test results is paramount. Laboratories implement rigorous quality control measures and validation processes:
- Internal Quality Control: Laboratories use control samples with known values to check the performance of their analysers. These control samples are tested alongside patient samples to ensure the machines are producing accurate results.
- External Quality Assessment: Laboratories participate in external proficiency testing programs, where they receive unknown samples to analyse. Their results are compared with those from other laboratories to ensure consistency and accuracy across different testing sites.
- Calibration: Regular calibration of instruments is performed using standards with known concentrations. Calibration ensures that the analysers provide accurate measurements over time.
- Technician Expertise: Skilled laboratory technicians and clinical pathologists play a crucial role in the analysis process. They review and validate the results, ensuring any anomalies are investigated and resolved. Their expertise is vital for interpreting complex data and providing accurate diagnostic information.
Common Tests and Their Analysis
Here are some common blood tests and how they are analysed:
- Complete Blood Count (CBC): Measures the number and types of blood cells. Anomalies in cell counts can indicate conditions such as anaemia, infection, and blood cancers.
- Basic Metabolic Panel (BMP): Includes tests for glucose, calcium, and electrolytes. It assesses kidney function and metabolic balance.
- Lipid Panel: Measures total cholesterol, LDL, HDL, and triglycerides. It evaluates cardiovascular risk and helps guide treatment for hyperlipidaemia.
- Liver Function Tests (LFTs): Measures liver enzymes (ALT, AST), bilirubin, and albumin. It helps diagnose liver diseases and monitor liver health.
- Thyroid Function Tests: Measures TSH, free T4, and free T3. It diagnoses hypo- or hyperthyroidism and monitors thyroid treatment.
The analysis of blood in the laboratory is a sophisticated process that combines cutting-edge technology with the expertise of trained professionals. From initial preparation and automated analysis to specialised techniques and stringent quality control, each step is meticulously designed to provide accurate and reliable results. These insights are crucial for diagnosing diseases, monitoring health conditions, and guiding effective treatment plans.
Think of the laboratory as a high-tech detective agency, using advanced tools and techniques to uncover vital clues about your health. With this detailed information, you and your healthcare provider can make informed decisions that support your overall well-being and long-term health.
Regularity Of Blood Tests
Determining the frequency of blood tests is a critical component of proactive health management. The regularity with which you should undergo blood testing depends on various factors, including your overall health, specific medical conditions, risk factors, and health goals. By tailoring the frequency of these tests to your individual needs, you can effectively monitor your health and catch potential issues early.
General Health Monitoring
For individuals without specific health concerns, an annual blood test is generally sufficient. This routine check-up helps establish baseline levels for various biomarkers and can detect early signs of potential health issues. Key tests often included in an annual health screening are:
- Complete Blood Count (CBC): Evaluates overall health and detects disorders such as anaemia and infections.
- Basic Metabolic Panel (BMP): Assesses kidney function, electrolyte balance, and blood glucose levels.
- Lipid Panel: Measures cholesterol and triglyceride levels to evaluate cardiovascular risk.
- Liver Function Tests (LFTs): Monitors liver health and detects liver disease.
- Thyroid Function Tests: Screens for thyroid disorders.
Annual testing provides a comprehensive overview of your health, allowing for timely interventions and lifestyle adjustments if necessary.
Monitoring Chronic Conditions:
For individuals with chronic health conditions, more frequent blood tests are essential to manage and monitor their condition effectively. The frequency of these tests depends on the specific condition and its severity:
- Diabetes: Regular monitoring of blood glucose levels and HbA1c is crucial. Typically, HbA1c tests are performed every 3 to 6 months to assess long-term glucose control and adjust treatment plans.
- Hypertension: Blood tests to monitor kidney function and electrolytes may be needed every 3 to 6 months, especially if on medication that affects these parameters.
- Hyperlipidaemia: For those on cholesterol-lowering medications, lipid panels are usually conducted every 3 to 6 months to ensure effectiveness and make dosage adjustments.
- Thyroid Disorders: Patients with hypo- or hyperthyroidism require thyroid function tests every 3 to 6 months to monitor hormone levels and adjust medication accordingly.
- Chronic Kidney Disease: Regular monitoring of kidney function (creatinine, eGFR) and electrolyte levels is necessary, often every 3 to 6 months.
Frequent testing helps manage these conditions more effectively, preventing complications and optimising treatment outcomes.
Performance and Athletic Goals
Athletes and fitness enthusiasts may benefit from more frequent blood tests to optimise performance and recovery. Testing every 3 to 6 months can help monitor:
- Haemoglobin and Hematocrit: Ensures adequate oxygen-carrying capacity and detects anaemia.
- Electrolytes: Maintains hydration and electrolyte balance, crucial for muscle function and endurance.
- Hormone Levels: Monitors testosterone, cortisol, and other hormones that influence performance, recovery, and overall health.
- Nutrient Levels: Checks for deficiencies in vitamins and minerals that can impact performance and recovery, such as iron, vitamin D, and magnesium.
Regular monitoring allows athletes to tailor their nutrition, training, and recovery strategies based on their specific needs.
Preventive Health and Risk Factors
Individuals with risk factors for certain conditions may require more frequent blood testing to monitor for early signs of disease:
- Family History of Heart Disease: Annual or bi-annual lipid panels and CRP tests can help detect early signs of cardiovascular disease.
- Risk of Diabetes: Those with pre-diabetes or a family history of diabetes may need blood glucose and HbA1c tests every 3 to 6 months.
- Cancer Surveillance: Individuals with a family history of certain cancers might benefit from regular screening for tumour markers, such as PSA for prostate cancer or CA-125 for ovarian cancer.
Preventive testing helps in early detection and timely intervention, potentially reducing the risk of serious health issues.
Age-Related Testing
As individuals age, the frequency and type of blood tests may change to address age-specific health concerns:
- Middle Age: Regular monitoring of lipid profiles, blood glucose, and thyroid function becomes more important to detect early signs of metabolic and cardiovascular diseases.
- Senior Years: More frequent testing for kidney function, liver function, and anaemia may be necessary, along with monitoring for chronic conditions like diabetes and hypertension.
Regular testing in older adults helps manage age-related health issues and maintain quality of life.
Personalised Testing Schedules
Ultimately, the frequency of blood tests should be personalised based on individual health needs and goals. Regular consultation with a healthcare provider is essential to determine the most appropriate testing schedule. Factors to consider include:
- Existing Health Conditions: Chronic diseases require more frequent monitoring.
- Family History: Genetic predispositions may necessitate regular screening.
- Lifestyle and Diet: Nutritional status and lifestyle choices can influence testing needs.
- Symptoms: Any new or worsening symptoms should prompt immediate testing.
The regularity of blood tests is a dynamic aspect of healthcare that should be tailored to your specific health needs and goals. Whether for general health monitoring, managing chronic conditions, optimising athletic performance, or preventive health, regular blood tests provide invaluable insights that guide effective health management.
Think of these tests as regular maintenance checks for your body, ensuring everything runs smoothly and addressing potential issues before they become major problems. By working closely with your healthcare provider, you can determine the optimal frequency of blood tests to support your long-term health and well-being.
Final Thoughts
In the quest for health, wellness, and performance, knowledge is power. Blood tests provide a wealth of information that can guide your decisions and help you live your best life. These tests reveal critical insights into various aspects of your health, from identifying nutrient deficiencies and monitoring chronic conditions to optimising athletic performance and detecting early signs of disease. By regularly monitoring your blood, you gain a deeper understanding of your body’s inner workings, allowing you to take proactive steps to maintain and improve your health.
Empowerment Through Knowledge
Blood tests empower you with the knowledge needed to make informed decisions about your health. They help you understand:
- Nutrient Levels: Identify and correct deficiencies that may impact your energy, mood, and overall well-being.
- Hormonal Balance: Monitor and manage hormone levels that influence everything from metabolism to mood regulation.
- Organ Function: Assess the health of vital organs like the liver and kidneys, ensuring they function optimally.
- Inflammation: Track inflammatory markers to prevent chronic diseases associated with long-term inflammation.
- Blood Glucose: Manage blood sugar levels to prevent or control diabetes, maintaining metabolic health.
- Cardiovascular Health: Monitor cholesterol and other markers to reduce the risk of heart disease and stroke.
Proactive Health Management
Regular blood tests enable proactive health management by:
- Early Detection: Catching potential health issues early, allowing for timely intervention and better outcomes.
- Personalised Care: Tailoring healthcare strategies to your unique needs and conditions, ensuring more effective treatment.
- Preventive Measures: Implementing lifestyle and dietary changes based on detailed insights, reducing the risk of developing chronic diseases.
- Monitoring Progress: Tracking the effectiveness of treatments and interventions, making necessary adjustments to achieve optimal results.
Holistic Approach
By integrating blood tests into your regular health routine, you adopt a holistic approach to wellness. This comprehensive perspective considers all aspects of your health, from physical and mental well-being to performance and preventive care. Regular blood testing acts as a foundation for this approach, providing the data needed to support every aspect of your health journey.
Living Your Best Life
Armed with the detailed information from blood tests, you can take control of your health and make choices that enhance your quality of life. Whether it’s adjusting your diet, optimising your exercise routine, managing stress, or addressing medical conditions, the insights gained from blood tests help you live a healthier, more vibrant life.
Actionable Steps:
- Schedule Regular Check-Ups: Make annual blood tests a part of your health routine. For specific conditions, follow your healthcare provider’s recommendations for more frequent testing.
- Consult with Professionals: Work with healthcare providers to interpret your test results and develop a personalised health plan.
- Stay Informed: Keep up-to-date with the latest health information and advances in blood testing to make informed decisions.
- Take Charge: Use the insights from blood tests to take proactive steps in managing your health, from lifestyle changes to medical treatments.
So, the next time you’re at the doctor’s office, consider rolling up your sleeve and taking a deeper look into the marvel that is you. Blood tests are more than just a diagnostic tool; they are a gateway to understanding and optimising your health. By leveraging the power of blood tests, you can transform your approach to wellness, ensuring a healthier, more fulfilling life. In the end, the knowledge gained from these tests truly becomes the power that drives your journey toward optimal health and performance.
